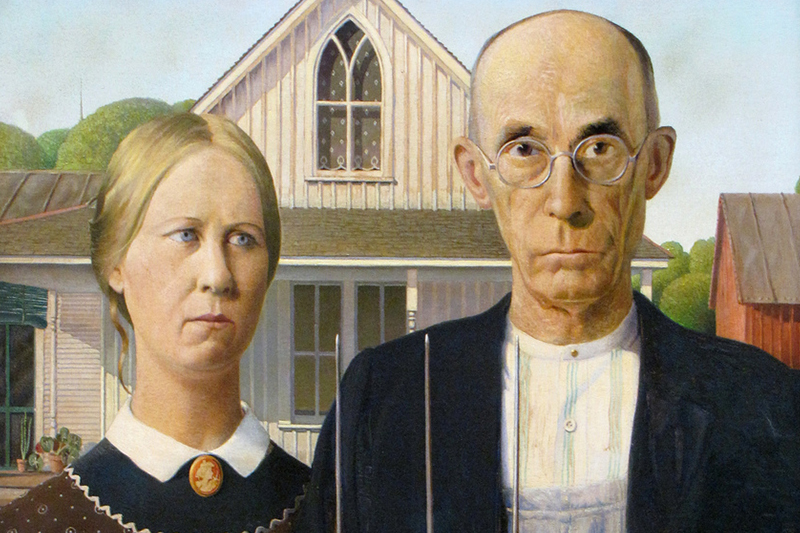
In the show, the main character Oliver Wendell Douglas (Eddie Arnold), ditches
his New York legal practice to become a farmer in rural America. Unfortunately,
today what Mr. Douglas would also experience with “farm livin’” is his access to
health care, and indeed his health might be at risk if he continued to live
there.
The landscape in small-town America might be bucolic, but the
health delivery system is not. “The health care delivery system in rural America
is largely fragmented, the rural health care workforce is stretched to its
limits in most states and rural households have higher rates of death,
disability and chronic disease. These challenges are significant because
approximately 51 million (1 in 6) people live in rural and frontier areas of the
country”*.
Some staggering statistics
from this organization:
- Despite only comprising 16 percent of the U.S. population, rural Americans reside in 75 percent of the total U.S. land area.[ii]
- Today, rural households have higher rates of death, disability and chronic disease.[iv]
- While nearly 85 percent of U.S. residents can reach a Level I or Level II trauma center within an hour, only 24 percent of residents living in rural areas can do so within that time frame.[vi]
- The rate of growth for seniors living in rural areas has tripled since the 1990s, and if the 80 million baby boomers living in the United States continue to follow these migration patterns, the rural population of those age 55 to 75 is set to increase 30 percent between 2010 and 2020. [viii]
- Of the 2,050 rural U.S. counties, 77 percent are designated as health professional shortage areas (HPSAs).[ix]
- Nearly 30 percent of rural primary care practitioners are at or nearing retirement age, while younger practitioners (those under age 40) account for only 20 percent of the current workforce.[x]
- Only 11 percent of physicians practice in rural America despite the fact that nearly one-fifth of the population lives in these areas.[xi]
- According to the U. S. Department of Health & Human Services, over 8,400 additional primary care providers are needed in rural America.[xii]
To make matters worse, hospitals- the main source of health services in urban and rural communities- are closing at an alarming rate.
- Eighty-nine rural hospitals have closed since 2010, and those closures are spread across 26 states, according to research from the North Carolina Rural Health Research Program.
- Across the U.S., more than 600 rural hospitals are vulnerable to closure, according to an estimate from iVantage Health Analytics.
- Of the states that have seen at least one rural hospital close since 2010, those with the most closures are in the South. Fifteen hospitals in Texas have closed since 2010, the most of any state. Tennessee has seen the second-most closures, with nine hospitals closing since 2010. In third place is Georgia with seven closures, followed by Alabama, Mississippi, North Carolina and Missouri, which have each seen five hospitals close over the past eight years.
County hospital ownership has vanished quicker than a bad crop. For-profit
hospital corporations that focused on rural (non-urban) health care delivery
accounted for nearly 40% of the closures between 2013 and 2017, according to a
report released in September by the U.S. Government Accountability Office. These
entities that focused on these demographics are in tremendous turmoil.
Bankruptcies, closures, fire sales to meet debt obligations, mergers and
acquisitions are changing this landscape and bringing more uncertainty to the
health picture for these communities.
So, what we have now almost a
quarter of the way into the 21st century is a growing rural population that is
older, poorer, not healthy and lacking in the basic healthcare options their
urban counterparts take for granted.
Creative answers are needed, as is
entrepreneurship. For example, here is one “creative” approach to keeping a
rural hospital open- at least in the short term while they grapple with a more
permanent solution.
According to the Enid News and Eagle, Pauls Valley
Regional Medical Center (Oklahoma) is soliciting donations from residents with
high net worth, including country music star Toby Keith, as officials look for a
long-term solution to the hospital's financial troubles. Donors have contributed
about $200,000 to the hospital, of which $4,000 came from a GoFundMe campaign,
according to the report**.
While this
approach is not sustainable, maybe another high net worth option could
be.
Could Wal Mart have an
answer?
Wal Mart- the bastion of retailing in
small town America, might be on the right path with their solution. They
recently announced that they would open “Town Centers” in their parking lots
which could include health clinics. Wal Mart is also partnering in Louisiana
with a regional medical health system (Ochsner) to launch a health insurance
plan for 6,600 Wal Mart and Sam’s Club employees.
Should Dollar General be thinking about how
they might be a bridge to better health for their
customers?
Steps like this with well-known rural
businesses might be able to bring medicine and affordable healthcare to this
segment of America.
More ambulatory facilities- taking medicine to where
you live- is another option. Broadening the ability for hospitals to qualify for
Critical Access definition is another step that should be discussed. Some have
stated that an expansion of state Medicaid programs is the answer to high levels
of uncompensated care that cripples rural hospitals.
Also, to keep costs
down and options open, rural healthcare providers need to address their
challenges as to what fits best in their environment. Many healthcare suppliers
(like CMS Imaging) are particularly nimble and offer affordable options that
scale in this application. What might be the choice in the big city often
doesn’t often scale as well out in the country?
Telemedicine could be an
answer as well. A short definition of telemedicine is the remote delivery of
healthcare via telecommunications technology. This segment of healthcare is
rapidly growing as an alternative to in-person practitioners. Remote cardiac
monitoring is an example of telemedicine. Consulting with a specialist over the
internet is another application. As telecommunications starts to pervade even
the most rural addresses, these types of systems or apps may be the key in
keeping patients in these zip codes healthier and out of emergency rooms that
are dozens of miles away. The ubiquitous iPhone might be the short-term
substitute for costlier urban care options.
The Rural health crisis is
real and getting more urgent every passing month. It demands increased attention
from policymakers, advocates, the media and entrepreneurs. Technology could
ultimately be the key.
While climbing a telephone pole for Eddie Arnold
to answer his phone was inconvenient, it shouldn’t be life-threatening. Maybe,
there could be an app for that soon.
- * Ncsl.org. (2018). Rural Health in America: Challenges and Opportunities for State Legislators. [online] Available at: http://www.ncsl.org/research/health/rural-health-challenges-and-opportunities.aspx [Accessed 12 Nov. 2018].
- ** Monies, P. (2018). Hospital's struggles reflect challenges rural hospitals face. [online] Enid News & Eagle. Available at: https://www.enidnews.com/news/local_news/hospital-s-struggles-reflect-challenges-rural-hospitals-face/article_3a631262-68d3-56ee-a041-877f64722d21.html [Accessed 12 Nov. 2018].








 ©
- CMS Imaging, Inc. All Rights
Reserved
©
- CMS Imaging, Inc. All Rights
Reserved

Comments
Jeff Z.
Savannah, GA
John,
Wednesday, November 15, 2018Interesting article and growth statistics serving rural areas across this country. I worked in a few of these rural healthcare facilities early in my career. I remember it being hard keeping up with technology and trying to provide all the services to meet demands and expectations of the communities we served. It is even harder today with ever shrinking reimbursements, high labor costs and regulatory IT demands. Just the IT demands and associated costs alone are staggering even for urban centers.
Often we asked for donations from a wealthy philanthropist or prominent family that could afford to occasionally help out. But as it is pointed out in your article this is not a sustainable strategy unless you have accessibility to a billionaire (S) with never ending roots in the community. It cost money to just survive operating a healthcare facility today and often wants of the community exceeds the ability to afford. I don't know if the Wal-Mart's, Amazons, CVS or other large retail operations will step up and save the rural access facilities across the nation. What I do know is that profitability counts and is the key to sustainability and survival. In the end as we all age reasonable access to good healthcare it is definitely something to think about when selecting a place to settle for good. Thanks for your thoughts.
P.S. I always got a kick out of Mr. Haney and Arnold the pig.
Leave a Comment